The Thinnest Person: Unveiling The Health Realities And Risks
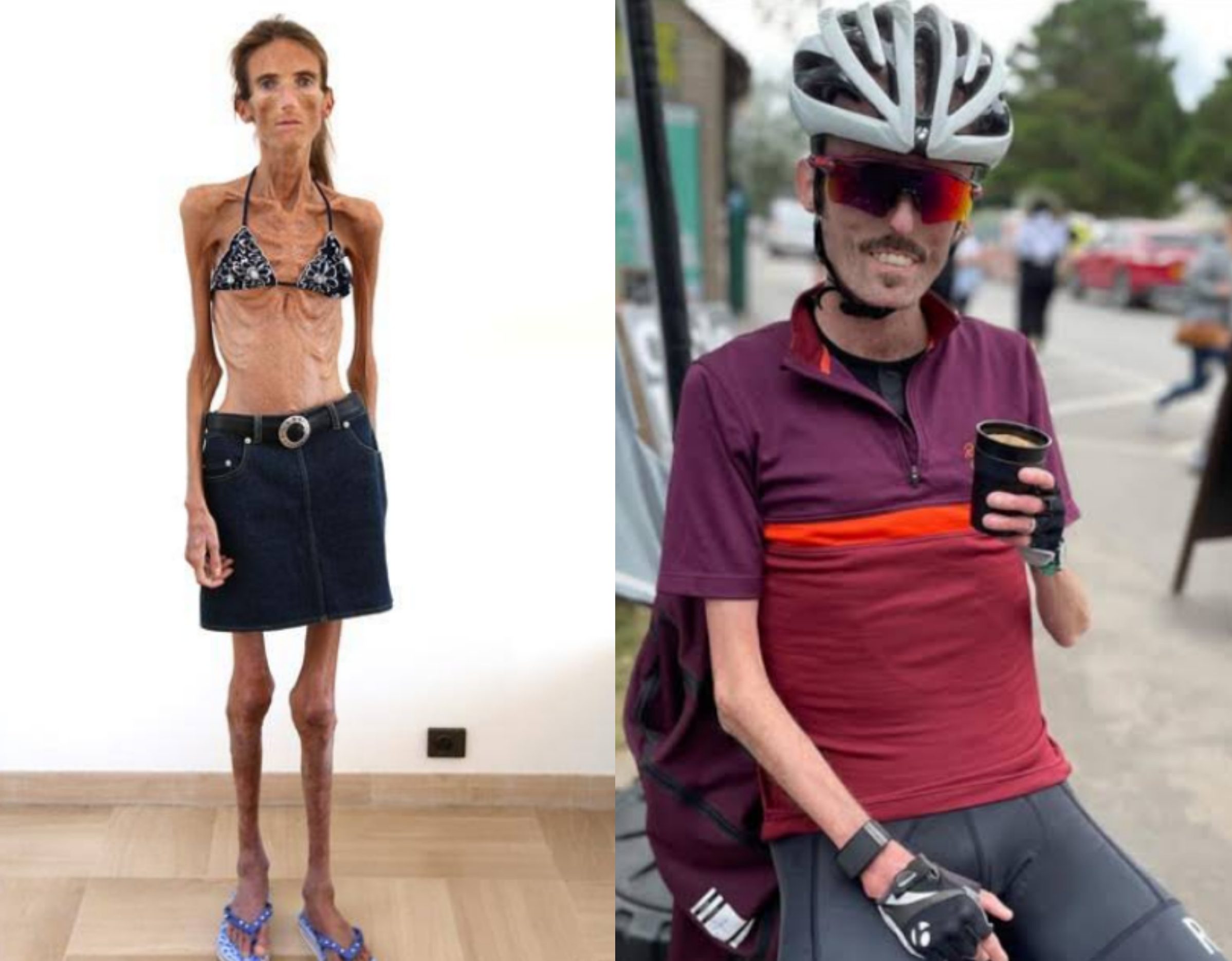
The concept of the "thinnest person" often conjures images that range from fascination to concern, yet beneath the surface lies a complex tapestry of health realities and profound risks. While media sometimes sensationalizes extreme body types, it's crucial to understand that being the thinnest person is rarely a testament to health or vitality. Instead, it frequently signals underlying medical conditions, severe malnutrition, or mental health struggles that demand serious attention and compassionate understanding. This article delves into what it truly means to be extremely thin, exploring the causes, the devastating health impacts, and the critical importance of a holistic approach to well-being.
Far from being a goal to aspire to, extreme thinness, particularly when it falls significantly below a healthy Body Mass Index (BMI), can be a life-threatening condition. It is not merely about aesthetics; it is about the fundamental functioning of the human body and mind. We will explore the various factors that contribute to such a state, from chronic illnesses and genetic predispositions to the pervasive influence of eating disorders. Our aim is to shed light on the severe consequences that accompany this extreme state, emphasizing why it’s imperative to shift the conversation from superficial appearance to genuine health and comprehensive care.
Table of Contents
- Defining Extreme Thinness: More Than Just a Number
- The Complex Causes Behind Extreme Thinness
- The Devastating Impact on Physical Health
- The Overlooked Role of Oral Health in Extreme Thinness
- Psychological and Emotional Toll of Extreme Thinness
- The Path to Recovery: Comprehensive Care
- Dispelling Myths and Promoting Healthy Body Image
- Seeking Help: Resources and Support
- Conclusion
Defining Extreme Thinness: More Than Just a Number
When we talk about the "thinnest person," we're often referring to individuals whose body weight is significantly below what is considered healthy for their height. The most common tool used to assess this is the Body Mass Index (BMI), a simple calculation derived from an individual's weight and height. While BMI is not a perfect measure and doesn't account for body composition (muscle vs. fat), it serves as a widely accepted screening tool for weight categories.
According to the World Health Organization (WHO), a BMI below 18.5 is classified as underweight. Extreme thinness, however, goes beyond just being underweight. It typically refers to a BMI of 17.0 or less, which is indicative of severe thinness, or even lower, pointing to profound malnutrition. For context, here's a general classification:
| BMI Category | BMI Range (kg/m²) | Health Implications |
|---|---|---|
| Severe Thinness (Grade III) | < 16.0 | Extremely high risk of health problems, severe malnutrition, organ damage. |
| Moderate Thinness (Grade II) | 16.0 – 16.9 | High risk of health problems, significant malnutrition. |
| Mild Thinness (Grade I) | 17.0 – 18.4 | Increased risk of health problems, potential nutrient deficiencies. |
| Normal Weight | 18.5 – 24.9 | Generally considered healthy weight range. |
| Overweight | 25.0 – 29.9 | Increased risk of certain health problems. |
| Obese | ≥ 30.0 | High risk of various chronic diseases. |
Being the thinnest person in a group, or even globally, often means falling into the severe thinness category, a state that carries immense health risks. It's a critical indicator that the body is not receiving adequate nourishment or is unable to process nutrients effectively, leading to a cascade of systemic failures. This condition is far from a benign state; it's a medical emergency that requires immediate and comprehensive intervention.
The Complex Causes Behind Extreme Thinness
The journey to becoming the thinnest person is rarely straightforward. It's often the culmination of a complex interplay of genetic predispositions, chronic diseases, psychological factors, and environmental influences. Understanding these root causes is fundamental to addressing the condition effectively and compassionately.
Medical Conditions and Chronic Illnesses
A significant number of individuals who are extremely thin are battling underlying medical conditions that hinder their ability to gain or maintain weight. These can include:
- Hyperthyroidism: An overactive thyroid gland can significantly boost metabolism, leading to rapid weight loss despite a normal or increased appetite.
- Gastrointestinal Disorders: Conditions like Crohn's disease, ulcerative colitis, celiac disease, or chronic pancreatitis impair the body's ability to absorb nutrients, leading to malabsorption and weight loss.
- Cancer: Many types of cancer, particularly in advanced stages, can cause cachexia – a complex metabolic syndrome characterized by severe weight loss, muscle wasting, and fatigue, often due to altered metabolism and loss of appetite.
- Chronic Infections: Persistent infections such as tuberculosis, HIV/AIDS, or parasitic infections can deplete the body's energy reserves and lead to significant weight loss.
- Diabetes (Type 1, uncontrolled): In uncontrolled Type 1 diabetes, the body cannot use glucose for energy and starts breaking down fat and muscle, leading to weight loss.
- Chronic Obstructive Pulmonary Disease (COPD): The increased effort required for breathing in severe COPD can burn a significant number of calories, contributing to weight loss.
These conditions require precise medical diagnosis and management, as addressing the underlying illness is the primary step towards healthy weight restoration.
Eating Disorders: Anorexia Nervosa
Perhaps one of the most widely recognized causes of extreme thinness, especially in the context of psychological factors, is Anorexia Nervosa. This severe eating disorder is characterized by an intense fear of gaining weight, a distorted body image, and self-starvation or excessive exercise leading to dangerously low body weight. Individuals with anorexia often perceive themselves as overweight even when they are critically underweight, striving to become the thinnest person they can be.
- Psychological Roots: Anorexia is not just about food; it's a complex mental illness often linked to perfectionism, anxiety, depression, low self-esteem, and a desire for control in other aspects of life.
- Behavioral Manifestations: Restricting food intake, obsessive calorie counting, compulsive exercise, purging behaviors (vomiting, laxative misuse), and abuse of diet pills are common.
- High Mortality Rate: Anorexia Nervosa has one of the highest mortality rates of any psychiatric illness, primarily due to medical complications arising from starvation and suicide.
Treatment for anorexia requires a comprehensive, multidisciplinary approach involving medical stabilization, nutritional rehabilitation, and extensive psychological therapy.
Socioeconomic Factors and Malnutrition
In many parts of the world, extreme thinness is a tragic consequence of poverty, food insecurity, and lack of access to nutritious food. Malnutrition, especially chronic undernutrition, can lead to severe wasting, particularly in children, making them incredibly vulnerable to illness and developmental delays. This is not about being the thinnest person by choice, but by circumstance.
- Food Scarcity: Insufficient access to food due to economic hardship, conflict, or natural disasters.
- Poor Dietary Diversity: Even when food is available, it may lack essential macronutrients and micronutrients, leading to deficiencies that impair growth and overall health.
- Inadequate Sanitation: Poor sanitation can lead to recurrent infections, which further deplete the body's nutritional reserves.
Addressing these factors requires large-scale humanitarian efforts, sustainable development, and public health initiatives focused on food security and improved living conditions.
The Devastating Impact on Physical Health
The human body is remarkably resilient, but prolonged extreme thinness pushes its systems to their breaking point. When the body is starved of essential nutrients, it begins to cannibalize its own tissues for energy, leading to widespread damage. The consequences of being the thinnest person can be severe and life-threatening, affecting virtually every organ system.
- Cardiovascular System: The heart, a muscle, shrinks and weakens. This can lead to dangerously low blood pressure, slow heart rate (bradycardia), arrhythmias (irregular heartbeats), and even heart failure. The risk of sudden cardiac death is significantly elevated.
- Skeletal System: Bone density decreases rapidly, leading to osteopenia and osteoporosis. This makes bones brittle and highly susceptible to fractures, even from minor falls. This damage can be irreversible.
- Endocrine System: Hormonal imbalances are rampant. In women, menstruation often ceases (amenorrhea), indicating a disruption in reproductive hormones. Thyroid function can slow down, and cortisol levels may rise, impacting metabolism and stress response.
- Gastrointestinal System: Digestion slows significantly, leading to constipation, bloating, and abdominal pain. The stomach may empty more slowly, causing early satiety and further reducing food intake.
- Renal System: Kidney function can be impaired, potentially leading to kidney failure due to dehydration and electrolyte imbalances.
- Immune System: A severely compromised immune system makes individuals highly susceptible to infections, from common colds to life-threatening pneumonia, as the body lacks the resources to fight off pathogens.
- Neurological System: Brain function can be affected, leading to difficulties with concentration, memory, and decision-making. Peripheral neuropathy (nerve damage) can cause numbness and tingling in the extremities.
- Skin, Hair, and Nails: Skin becomes dry, flaky, and may develop a fine, downy hair called lanugo as the body tries to conserve heat. Hair becomes brittle and falls out, and nails become weak and break easily.
These physical tolls underscore that extreme thinness is a critical medical emergency, demanding immediate and expert intervention to prevent irreversible damage and save lives.
The Overlooked Role of Oral Health in Extreme Thinness
While the more dramatic impacts of extreme thinness on vital organs often take center stage, the health of the mouth and teeth, often overlooked, is a crucial component of overall well-being. Indeed, in the broader context of health, oral health is increasingly recognized as an important component of general health, involving complex biological processes where various aspects converge. This is particularly true for individuals struggling with severe malnutrition or eating disorders, where the systemic compromises profoundly affect oral tissues.
The topic of oral health has gained significant relevance in academic and political circles, with important strategies being applied to address needs and problems. The loss of oral health presents itself through various diseases and conditions, among which dental caries and periodontal diseases stand out due to their high prevalence. In fact, oral diseases are among the most widespread non-communicable diseases globally, affecting an estimated 3.5 billion people. For someone who is the thinnest person, these issues can be exacerbated and have unique manifestations.
Here’s how extreme thinness and its underlying causes can impact oral health:
- Increased Risk of Dental Caries (Cavities): Malnutrition weakens tooth enamel, making it more susceptible to decay. Additionally, for individuals with eating disorders, frequent vomiting (a common purging behavior in bulimia and some forms of anorexia) exposes teeth to stomach acid, which erodes enamel. This erosion, combined with poor nutrition, creates a perfect storm for cavities.
- Periodontal Diseases (Gum Disease): The immune system is severely compromised in individuals with extreme thinness. This makes them more vulnerable to infections, including those that cause gingivitis and periodontitis. Gums may become inflamed, bleed easily, and eventually, the supporting bone structure around teeth can be destroyed, leading to tooth loss.
- Dry Mouth (Xerostomia): Dehydration, common in individuals with extreme thinness or those with eating disorders, reduces saliva production. Saliva is crucial for washing away food particles, neutralizing acids, and remineralizing enamel. A dry mouth significantly increases the risk of both caries and gum disease.
- Enamel Erosion: As mentioned, recurrent vomiting in conditions like Anorexia Nervosa leads to severe erosion of tooth enamel, particularly on the lingual (tongue-side) surfaces of the front teeth. This can cause sensitivity, changes in tooth shape, and increased risk of fracture.
- Nutrient Deficiencies: A lack of essential vitamins and minerals (e.g., Vitamin C for gum health, Vitamin D and Calcium for bone and tooth structure) directly impacts the health of oral tissues, making them fragile and slow to heal.
- Swollen Salivary Glands: In some cases, particularly with bulimia or purging anorexia, the salivary glands (especially the parotid glands) can become swollen, giving the appearance of chipmunk cheeks.
In this context, a review of the current concept of oral health, the impact of oral diseases on our population, and risk behaviors in oral health becomes crucial. Healthcare teams need to be equipped to promote oral health, prevent major detected oral diseases, and intervene effectively. This includes appropriate oral care practices, the effective use of fluoride, and healthy lifestyle habits related to diet, nutrition, personal hygiene, and the reduction of risk factors. For someone struggling with extreme thinness, integrating oral health care into their overall treatment plan is not just beneficial, but essential for a comprehensive recovery and improved quality of life.
Psychological and Emotional Toll of Extreme Thinness
Beyond the visible physical deterioration, being the thinnest person often comes with a heavy psychological and emotional burden. The mind and body are intricately connected, and the severe physical stress of extreme thinness profoundly impacts mental well-being. This is particularly true for individuals whose extreme thinness stems from eating disorders, where psychological distress is both a cause and a consequence.
- Co-occurring Mental Health Conditions: A high percentage of individuals with eating disorders or severe malnutrition also suffer from other mental health conditions. These often include depression, anxiety disorders (including generalized anxiety, social anxiety, and obsessive-compulsive disorder), and personality disorders. These conditions can exacerbate the eating disorder and complicate recovery.
- Body Image Distortion: A hallmark of anorexia nervosa is a severely distorted body image. Even when dangerously underweight, individuals may perceive themselves as fat or believe certain body parts are too large. This distortion fuels the drive to become even thinner, perpetuating the cycle of self-starvation.
- Cognitive Impairment: Starvation affects brain function, leading to difficulties with concentration, memory, and problem-solving. This "brain fog" can make it challenging for individuals to engage in therapy or make sound decisions about their health.
- Social Isolation: The secrecy, shame, and rituals associated with extreme thinness or eating disorders often lead to social withdrawal. Individuals may avoid social gatherings, especially those involving food, leading to profound loneliness and isolation.
- Irritability and Mood Swings: Malnutrition can cause significant mood dysregulation, leading to increased irritability, emotional lability, and a general sense of hopelessness.
- Obsessive Thoughts: Thoughts about food, weight, and body shape can become all-consuming, dominating daily life and making it difficult to focus on anything else.
Addressing these psychological dimensions is as crucial as physical rehabilitation. True recovery for the thinnest person necessitates comprehensive mental health support.
The Path to Recovery: Comprehensive Care
Recovery from extreme thinness, especially when it is a result of complex medical or psychological conditions, is a challenging but achievable journey. It requires a holistic, patient-centered approach that addresses both the physical and mental aspects of the condition. There is no quick fix; rather, it is a gradual process of healing and re-establishing a healthy relationship with food and body.
Multidisciplinary Approach
Effective treatment for individuals who are extremely thin typically involves a team of specialists working collaboratively. This multidisciplinary approach ensures that all facets of the condition are addressed comprehensively:
- Medical Doctor/Physician: Responsible for medical stabilization, monitoring vital signs, addressing physical complications (e.g., cardiac issues, electrolyte imbalances, bone density loss), and managing any underlying medical conditions.
- Registered Dietitian/Nutritionist: Crucial for nutritional rehabilitation. They develop individualized meal plans, educate on healthy eating, challenge food fears, and guide weight restoration in a safe and sustainable manner.
- Psychologist/Therapist: Provides psychotherapy (e.g., Cognitive Behavioral Therapy, Family-Based Treatment, Dialectical Behavior Therapy) to address the underlying psychological issues, distorted body image, co-occurring mental health conditions, and behavioral patterns associated with extreme thinness.
- Psychiatrist: May be involved to assess and manage any psychiatric comorbidities, such as depression, anxiety, or OCD, often through medication if appropriate.
- Dentist/Oral Health Professional: As discussed, oral health is a vital part of general health. A dentist can address issues like enamel erosion, caries, and gum disease, which are prevalent in individuals with extreme thinness, particularly those with eating disorders.
- Social Worker/Case Manager: Helps navigate practical challenges, coordinates care, and connects individuals and families with support resources.
This integrated approach ensures that the individual receives comprehensive care, from immediate medical needs to long-term psychological and nutritional support, paving the way for sustainable recovery for the thinnest person.
Nutritional Rehabilitation
One of the most critical components of recovery is nutritional rehabilitation, which aims to safely restore a healthy weight and correct nutritional deficiencies. This process must be carefully managed to avoid refeeding syndrome, a potentially fatal shift in fluids and electrolytes that can occur when severely malnourished individuals are re-fed too quickly.
- Gradual Reintroduction of Food: Calories are increased slowly and steadily to allow the body to adapt.
- Balanced Macronutrients and Micronutrients: Focus is placed on providing a balanced diet rich in carbohydrates, proteins, fats, vitamins, and minerals essential for bodily function and repair.
- Regular Meal Patterns: Establishing consistent meal and snack times helps to normalize eating behaviors and regulate metabolism.
- Addressing Food Fears: A dietitian helps individuals confront and overcome their fears surrounding specific foods or food groups.
Nutritional rehabilitation is not just about gaining weight; it's about restoring physical health, cognitive function, and the body's ability to heal and thrive.
Dispelling Myths and Promoting Healthy Body Image
In a society often obsessed with appearance, there's a pervasive misconception that being the thinnest person equates to peak health, beauty, or success. This dangerous myth is perpetuated by media portrayals, social media trends, and a lack of understanding about true health. It's crucial to actively dispel these myths and promote a culture that values health, well-being, and body diversity over unrealistic ideals.
- Health is Not a Size: True health encompasses physical, mental, and emotional well-being, none of which are dictated by a specific number on a scale or a clothing size. A person can be thin and unhealthy, just as a person can be larger and healthy.
- Challenging Glorification: It's vital to challenge any narrative that glorifies extreme thinness. Such portrayals can be highly triggering for individuals struggling with eating disorders and can contribute to a societal pressure to achieve an unhealthy body type.
- Media Literacy: Educating ourselves and others on how media constructs and perpetuates unrealistic body ideals is important. Understanding that images are often manipulated or represent an unachievable standard can help foster a more critical perspective.
- Focus on Function, Not Appearance: Shifting the conversation from how bodies look to what bodies can do (e.g., move, create, connect) can foster a more positive and appreciative relationship with one's body.
- Promoting Body Neutrality and Positivity: Encouraging acceptance of one's body as it is, and fostering respect for all body types, is key to building a healthier society. Body neutrality focuses on the body's functions rather than its appearance, while body positivity actively celebrates diverse body shapes and sizes.
By promoting a more balanced and realistic view of health and body image, we can create an environment that supports recovery for those struggling with extreme thinness and prevents others from falling into its dangerous traps. The goal should never be to be the thinnest person, but the healthiest
Skinniest Person: Meet 10 World's Thinnest People Alive 2024 - The

Discovering The Thinnest Person In The World: A Journey Through Facts

Who is the thinnest person in the world alive? - ABTC